Alright, let’s talk about something that was a huge question mark for me, and I bet for a lot of you going through the whole IVF rollercoaster: can you have sex after an embryo transfer? Man, the things they don’t explicitly tell you, or tell you in such a roundabout way, it’s enough to make your head spin.
My Journey Down the Rabbit Hole
So, there I was, post-transfer. You know the drill. You’re pumped full of hormones, you’ve got this tiny little speck of hope inside you, and suddenly your body feels like it’s not even yours anymore. It’s like, public property for the doctors, and a super delicate, fragile vessel for you. I remember getting a whole list of “don’ts” from my clinic. It was intense.
- Don’t lift anything heavy. What’s heavy? Is my laptop heavy? My cat?
- Don’t take hot baths or go in saunas. Okay, that one made sense.
- Don’t do strenuous exercise. Again, what’s “strenuous”? Is walking up the stairs too fast strenuous?
- And a whole bunch of other stuff that just added to the anxiety.
I swear, I was analyzing every single thing I did. I became this super cautious person, tiptoeing around my own life. My husband, bless him, was trying to be supportive but he was just as clueless and worried as I was. We were both walking on eggshells, literally and figuratively.
The Elephant in the Room
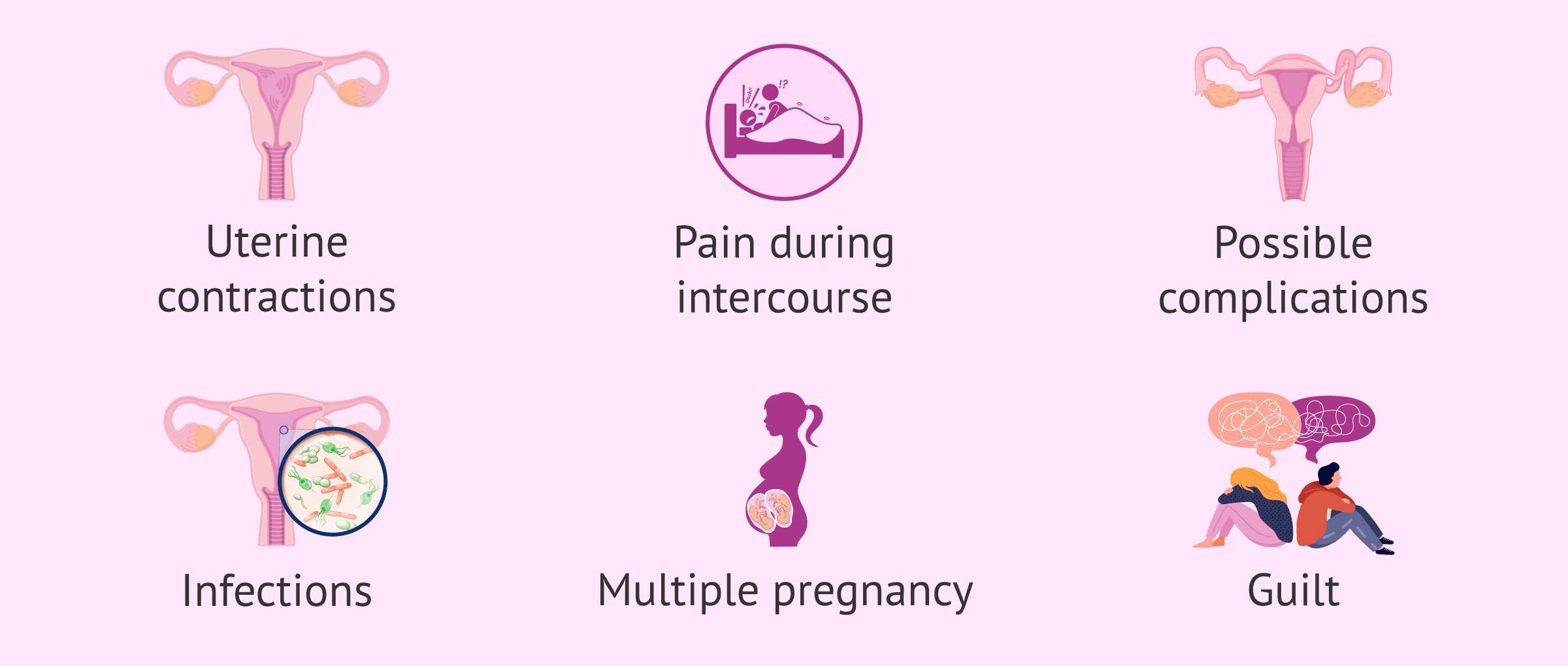
Then, the “sex” question popped into my head. It wasn’t really on the clinic’s main list of “don’ts,” not explicitly anyway. Some pamphlets vaguely mentioned “pelvic rest,” but what did that even mean? Was it just for a day? A week? Until the pregnancy test? Forever? Okay, maybe not forever, but you get my drift. The ambiguity was killing me.
I did what we all do, right? I tried to casually ask my nurse during one of the check-ins. She was a bit vague, said something like, “Well, some doctors say abstain, some say it’s fine after a few days, maybe just be gentle.” Super helpful, right? Not. It felt like nobody wanted to give a straight answer. It was like asking about the meaning of life during a very specific, very delicate medical procedure.
And of course, I peeked online. Oh boy. That was a mistake. Some people were adamant: “Absolutely not! You’ll mess everything up!” Others were like, “My doctor said it was fine, even good for blood flow!” And then there were the horror stories and the miracle stories all mixed together. It just made me more confused and anxious.
What We Ended Up Doing
So, here’s what we actually did. After all the hemming and hawing, and the vague advice, and my own internal panic, my husband and I talked. A lot. We were both stressed, both hopeful, and honestly, both a bit scared of doing anything “wrong.”
We decided to wait. Yeah, that was our big “practice.” We chose to err on the side of extreme caution. For us, the mental peace of knowing we hadn’t done anything that could (in our worried minds) jeopardize things was more important than anything else at that moment. We waited through the whole two-week wait (which felt like two years, by the way). We figured, we’ve come this far, put our bodies and emotions through so much, what’s another couple of weeks of just… being careful?
Was it the “right” decision? Medically? I still don’t know for sure. There’s no big study I can point to that definitively says our choice was the magic key. But for us, in that specific moment, with our specific anxieties, it felt like the right path.
Looking Back
Honestly, the whole IVF process is such a mind game. Every little thing feels monumental. That period after the transfer is particularly brutal because you’re in limbo. You’re pregnant until proven otherwise, but also, not really pregnant yet. It’s a weird, stressful place to be.
My advice, if I can even call it that, isn’t about whether you should or shouldn’t. It’s more about communicating with your partner and trying to get the clearest possible information from your clinic. If they’re vague, press them. Ask them to explain their reasoning. And then, you and your partner have to decide what feels right for you. What will give you the most peace of mind during an already incredibly stressful time? For us, it was abstaining. For someone else, it might be different, and that’s okay too.

The main thing I learned? You have to be your own advocate, and sometimes, you just have to make the decision that lets you sleep a little better at night, even if it’s based more on gut feeling and managing anxiety than on hard science. It’s a tough road, this IVF thing.